Glaucoma is a chronic eye condition in which elevated eye pressure leads to slow but progressive damage of the optic nerve (nerve of sight) causing loss of peripheral vision in the early stages and if left untreated gradually encroaches to affect the central vision in the late stages. Unfortunately, the visual loss from glaucoma is not reversible and may lead to permanent visual impairment. However, the good news is that glaucoma can be effectively treated to preserve vision and prevent permanent loss of vision by lowering the eye pressure which delays further damage to the optic nerve. Screening for glaucoma is recommended in patients with a higher risk (positive family history, Black ethnicity) after the age of 40 and this can be done during a routine eye test at the optician’s on a yearly basis.
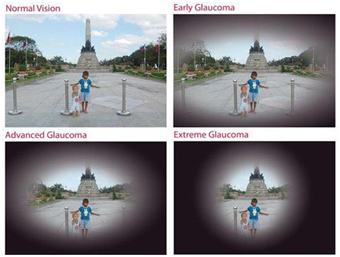
The vast majority of patients usually don’t experience any initial symptoms in the early stages and symptoms only become apparent in the late stages of the condition when blurriness of the side vision may be reported. The central vision is preserved until the very end (‘tunnel vision’).
A very small minority of patients may rarely present with acute symptoms of a painful red eye with cloudy vision when the eye pressure is severely elevated which requires emergency treatment. This is referred to as an ‘acute attack of glaucoma’.
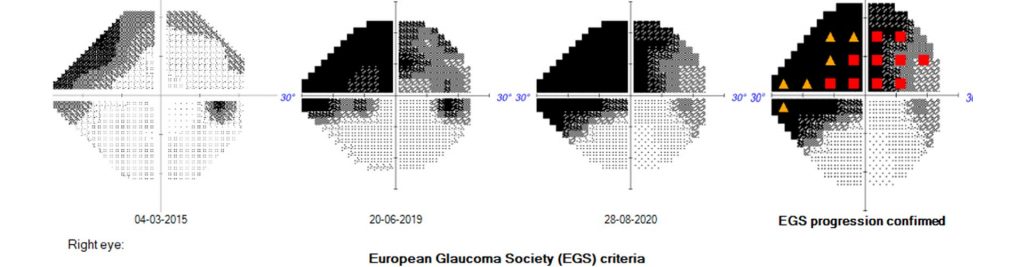
Opticians will refer patients to an ophthalmologist if there is suspicion of elevated eye pressure during a routine eye test. The ophthalmologist reconfirms the elevated eye pressure, assesses the clinical appearance of the optic nerve at the back of the eye and reviews the formal visual field test for any abnormalities (‘defects or scotoma’) based on which a confirmed diagnosis of glaucoma is made.
Majority of patients have ‘primary open angle glaucoma’ (POAG) where the ‘drainage angles’ of the eye between the peripheral iris tissue (blue or brown coloured part of the eye) and cornea are open but there is resistance to the outflow of fluid leading to elevated eye pressure which cause optic nerve damage over time (usually several years).
A minority of patients have ‘primary angle closure glaucoma’ (PACG) where the ‘drainage angles’ are narrow or semi-closed causing mechanical obstruction to the outflow of fluid leading to elevated eye pressure. Very rarely, in this group of patients if the drainage angles get completely closed it may lead to acutely elevated very high eye pressure when it’s called ‘an attack of primary angle closure’ .
Normal tension glaucoma is a type of open angle glaucoma where the eye pressure is within the ‘normal range’ but high enough to cause damage to the optic nerve for that particular eye.
In primary congenital glaucoma babies can be born with poor drainage angles.
Left untreated, glaucoma will progress from affecting the side vision in early stages to affecting the central vision in late stages (tunnel vision). The duration is variable depending on the level of elevated eye pressure from few years to several years. With appropriate treatment the progression can be delayed to help preserve vision for a long period of time (usually decades).
Treatment can be divided in 3 sections – medications (eye drops), laser treatment and surgery. Eye drops are very effective in the initial stages and more than one drop is often required to effectively achieve the ideal ‘target pressure’ which is determined by your ophthalmologist. The limitations with eye drop therapy are side effects, difficulty with compliance to regularly use drops over long periods of time and loss of effectiveness over time. Selective laser trabeculoplasty (SLT) is considered when eye drops are either inadequate or at an earlier stage on the advice of your ophthalmologist. Trabeculectomy filtration surgery is considered when the other treatment modalities have become ineffective.

Limitations of glaucoma drop therapy: Side effects include reaction of the ocular surface to the preservatives in the eye drops (used to increase shelf-life), difficulty with compliance in forgetful patients or patients with busy life style, natural loss of ‘adherence’ to use drops regularly over several years and loss of effectiveness over time.
Once eye drops start to lose its efficacy to adequately lower the eye pressure, laser treatment is usually the next resort for treating open angle glaucoma. Mr Bhatta offers different types of laser treatment for glaucoma in his clinic.

In BMI Albyn, the SLT laser is exclusively offered by Mr Bhatta as a specialised laser treatment for glaucoma. The suitability for SLT is best determined after proper assessment of the drainage angles of your eye by the consultant, since the laser may not be suitable for all eyes. Once confirmed and agreed to proceed with the SLT laser, this is undertaken as an outpatient clinic procedure.
How does SLT work? SLT is a gentle laser which is very safe for the eyes. The laser is delivered to the drainage angles or trabecular meshwork and is expected to facilitate the outflow of fluid leading to a lower eye pressure. The limitations are that SLT laser may not be effective in 20 – 30 % of patients and the effectiveness gradually wears off over time (usually after few years). However, due to its excellent safety profile it could be repeated in selected patients and patients who have had SLT previously can still qualify for other treatments including surgery in the future, if felt necessary by the consultant.
What to expect on the day of SLT laser treatment?
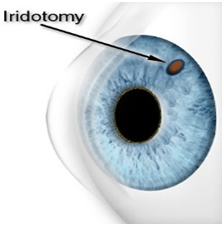
Mr Bhatta offers YAG laser peripheral iridotomy (PI) as a clinic procedure. Laser PI is commonly performed as a preventative measure for eyes with a narrow drainage angle which runs the risk of getting occluded and cause an attack of ’primary angle closure’. This can lead to an acute painful red eye with a very raised eye pressure. Longsighted (hypermetropic) eyes are at slightly higher risk. The laser iridotomy is a very safe treatment which carries a minimal risk (< 5 %) of glare in the long term especially in bright light but most patients cope well without problems.
Rarely, laser iridotomy is performed as an emergency treatment when an ‘attack of angle closure glaucoma’ has already occurred in a painful red eye with reduced vision due to elevated eye pressure. The patient automatically presents to the A&E in a hospital setting. Laser iridotomy in then carried out by the on-call ophthalmologist to treat the condition as a matter of urgency.
Commonly there may be no symptoms and your optician may pick up the signs of a ‘narrow drainage angle’ during a routine eye test and refer you to the ophthalmologist for further assessment if a laser peripheral iridotomy is necessary to reduce the risk of ‘an acute attack of glaucoma’ in the future. Less commonly, there may be associated symptoms of intermittent headaches, blurry vision or haloes.
What to expect on the day of laser Peripheral Iridotomy treatment?
Surgery will be recommended by Mr Bhatta when eye drops and laser treatment are inadequate to control your glaucoma satisfactorily. Trabeculectomy surgery is the gold standard invasive glaucoma filtration surgery.
Trabeculectomy can be performed alone or may be combined with a cataract surgery. Mr Bhatta prefers to perform cataract surgery ahead of trabeculectomy since this often lowers the eye pressure and may delay the need for more invasive trabeculectomy which is however not always the case. The operation takes less than an hour to perform (45 minutes) and can be safely performed under a local or general anaesthesia depending on patient’s preference.
A small flap of tissue is raised on the outer white coat (sclera) of the eye towards the top area of the eye-ball so that it remains covered under the upper eyelid. Mitomycin C, a special anti-scarring medicine is applied transiently to the local area and quickly washed off to improve the success rate of the operation. A tiny opening (< 1 mm) is then punched in the trabecular meshwork inside the eye and the scleral flap is repositioned back and secured with stitches. Most of the stitches dissolve and fall out on their own and some ‘releasable stitches’ may need to be removed in the first few weeks following the surgery which can be easily done during a clinic review consultation with Mr Bhatta.
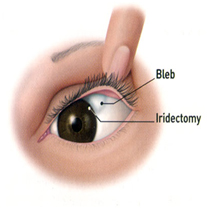
The final effect that can be expected is somewhat similar to a small blister (‘bleb’) on the surface of the eye tucked under the upper eyelid through which the outflow of fluid from inside the eye continues into the neighbouring circulation resulting in a lower eye pressure.
Frequent postoperative reviews are necessary with Mr Bhatta on a weekly or fortnightly basis for a couple of months in the immediate postoperative period to ensure that the operated eye is settling down well.
Postoperative care – DO’s and DON’Ts:
Various newer micro-invasive glaucoma surgeries have been widely accepted with in the UK and worldwide to treat glaucoma. Few of them are gaining increasing popularity amongst glaucoma surgeons and patients based on their safety profile and efficacy. The main advantage of MIGS is that these are ‘minimally invasive’ as the name suggests and can be conveniently performed in combination with a cataract surgery which may help delay the need for a more invasive surgery like trabeculectomy. Few of these MIGS have shown encouraging results.
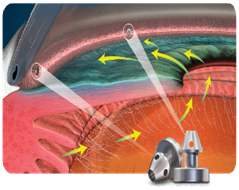
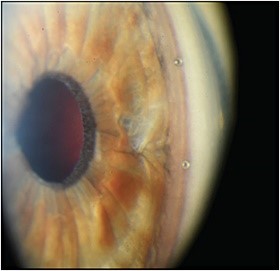
The iStent inject® and the Xen implant are two such MIGS devices that Mr Bhatta is equipped to perform on his glaucoma patients. Careful patient selection, appropriate counselling and realistic expectations are essential which Mr Bhatta would discuss in great detail on an individual patient basis before proceeding with these newer novel surgeries . MIGS are suitable for open angle glaucoma, usually of mild to moderate severity and can be conveniently combined with a cataract surgery or performed on its own as a stand alone procedure.
The iStent inject®:
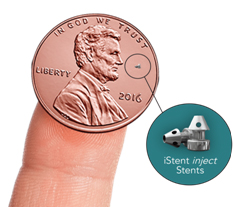
In Aberdeen, the iStent inject® is exclusively offered by Mr Bhatta for his glaucoma patients (unavailable in the NHS). The iStent inject® is the smallest medical device known to be implanted in the human body which has been CE marked in 2010 and FDA approved in 2018. It is only 0.36mm long and made of titanium. The device is implanted with the help of a pre-loaded injector system, very precisely into the trabecular meshwork (drainage angle) where it bypasses the obstruction of the natural drainage pathway to increase the outflow of fluid. The surgery takes an additional 15 – 20 minutes if combined at the end of a cataract surgery or approximately 30 – 35 minutes if performed as a stand-alone procedure and is carried out conveniently under a local anaesthesia just like a cataract surgery.
GDD is reserved for more complex and refractory glaucoma patients unresponsive to conventional treatments, laser procedure and trabeculectomy surgery or MIGS. Mr Bhatta will discuss this option at length with patient during clinic consultation when the need arises.
Glaucoma is a chronic condition which needs life-long monitoring on a regular basis. Mr Bhatta offers comprehensive and ongoing glaucoma monitoring services for his patients by checking the eye pressure, clinically assessing if there has been a change in the appearance of the optic nerve and analysing if there has been any progression in the visual field test or scans of the optic nerve. For stable glaucoma patients the monitoring is usually 6 monthly or yearly, for progressive glaucoma patients this may be more frequent. Depending on the rate of progression, a combination of different strategies described above are deployed for effective management of glaucoma which are best determined by the consultant.
NTG is associated with low intraocular pressure (less than 22 mm Hg). There are several associated risk factors implicated of which few are as below:
Additional special investigations like blood tests, MRI scans, optic nerve OCT scans are often required to confirm the diagnosis.
Treatment is mostly similar to primary open angle glaucoma, although it may be tricky since progression can continue despite low levels of eye pressure.
PEX glaucoma is one the commonest types of secondary open-angle glaucoma which can be seen in the white population, with a predilection for Scandinavian origin but also prevalent in other areas of the world. Family history may be present.
Although the exact cause of pseudoexfoliation is unknown, it is believed to be a systemic disorder usually affecting patients above 50 years of age. In PEX syndrome whitish granular ‘dandruff-like’ protein material is found to be deposited on the lens, iris, ciliary epithelium and cornea inside the front segment of the eye which are washed and deposited onto the trabecular meshwork by the natural flow of fluid inside the eye. This causes blockage of the drainage angle and raises the intraocular pressure. Similar exfoliative material can be found in other parts of the body like the skin, liver and kidneys, but are of reduced significance.
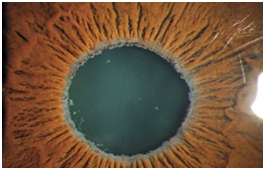
Signs and symptoms: The clinical signs are quite accurately identified on slit lamp examination during a clinic consultation by your ophthalmologist. Typical features are deposition of white flaky material on the border of the pupil and anterior surface of the lens (please see picture), with some degree of increased pigmentation of the anterior chamber angle (which could be narrow in 20% of pseudoexfoliatives). Commonly one eye is more affected than the other. Approximately 40 – 50% of patients with pseudoexfoliation will develop PEX glaucoma. So it’s important for patients with ocular signs of pseudoexfoliation to have their eye pressures monitored on a regular basis.
Treatment: PEX glaucoma is treated similar to primary open-angle glaucoma although the level of eye pressure can be much higher and the glaucoma can worsen at a faster pace. Hence, more aggressive treatment is often required. Selective laser trabeculoplasty (SLT) can be particularly effective in the earlier stages of the condition. Glaucoma surgery may be necessary to treat progressive PEX glaucoma.
PDS is a spectrum of uncommon eye condition where pigments from the back of the iris are released in certain individuals whose iris is bowed backward and predisposes it to rub against the crystalline natural lens which lies immediately behind it. Short-sighted younger individuals aged 30 to 50 years are typical candidates. Over years these released pigments get deposited on the back surface of the cornea (Krukenberg’s spindle) and the trabecular meshwork and may cause obstruction to outflow of fluid resulting in elevated eye pressure and causing pigmentary glaucoma which is a type of secondary open-angle glaucoma.
Treatment: Pigmentary glaucoma is treated similar to primary open-angle glaucoma. Selective laser trabeculoplasty can be particularly effective in treating pigmentary glaucoma and is one of the preferred methods of treating this condition. Additionally, studies have shown that creating a tiny opening in the corner of the iris tissue by performing a laser peripheral iridotomy often helps to minimise the pigment dispersion by reducing the posterior bowing of the iris and making the iris contour flatter, thereby minimising the long term risk of pigmentary glaucoma. Surgery may be necessary for treating progressive pigmentary glaucoma.
OHT refers to eye pressure elevated above the normal level (ie more than 21 mmHg). This is not classified as glaucoma due to the absence of optic nerve damage which must occur in order to define glaucoma. So, OHT could be described as ‘pre-glaucoma’ since it predisposes individuals to develop glaucoma over a period of time. The landmark Ocular Hypertension Treatment Study (OHTS) predicts the higher risk of developing glaucoma in OHT patients with an increased cup-disc ratio of the optic nerve, thinner corneas, age above 40 and Afro-Caribbean origin. Studies have shown there is a 10% risk of developing glaucoma in 5 years in patients with OHT.
Monitoring and treatment of OHT: In the absence of other risk factors and the presence of a healthy optic nerve and a normal visual field, OHT may be safely monitored without the need for treatment on the advice of your consultant ophthalmologist if the eye pressure is only modestly elevated (early to mid-20s mmHg). For others with consistently higher eye pressure (late-20s and above), OHT may warrant treatment to lower the eye pressure which reduces the risk of progression to glaucoma from 10% to 5% in 5 years, which is a 50% reduction of risk. Eye drops or selective laser trabeculoplasty can both be used effectively to treat OHT. A very small group of ocular hypertensives may need glaucoma surgery if eye pressure is severely elevated despite medical or laser treatment especially in the presence of other risk factors. It is recommended to consult an ophthalmologist for monitoring and treatment of OHT.
Glaucoma is the commonest cause of irreversible blindness affecting 80 million individuals worldwide in 2020. The overall prevalence is 3% for people aged 40 to 80 years (Lancet). In the UK approximately half a million people are diagnosed with glaucoma which means 1 in 150 people have the condition. The Royal College of Ophthalmologists have predicted in its ‘Way forward’ project that this number will rise by 44% between 2015 and 2035.
Elevated eye pressure and age are the two most important risk factors (above 50s and 60s) followed by a positive family history of glaucoma (parents or siblings). Amongst other risk factors are Afro-Caribbean ethnicity, diabetes, short-sightedness, steroid use and previous eye trauma to name a few of them.
Primary glaucoma
Primary open angle glaucoma (POAG) is the commonest form of glaucoma which develops in adulthood and may be associated with one or more of the risk factors. Pigment dispersion glaucoma and pseudoexfoliation glaucoma are also open-angle glaucoma but are secondary to other eye conditions.
Primary angle closure glaucoma (PACG) is the less common form where the drainage angle or trabecular meshwork is narrow or semi-closed due to the cornea and peripheral iris remaining in closer proximity of each other leading to obstruction of outflow of fluid. On rare occasion this can lead to an acutely painful red eye which needs to be treated urgently (within hours) by tablets, injections, eye drops and an urgent YAG laser peripheral iridotomy where by a small opening is created in the peripheral iris tissue which releases the hold up of fluid inside the eye and lowers the eye pressure instantaneously. Very often, a cataract extraction is necessary in due course which is nowadays considered to be the most important predisposing factor for the ‘acute attack of primary angle closure’ and a cataract surgery resolves the condition more permanently. Many patients with chronic angle closure glaucoma may still need long term eye drops or a trabeculectomy filtration surgery in the future.
Primary congenital glaucoma
(glaucoma during infancy or within first few years of life)
Developmental glaucoma
(glaucoma due to developmental anomalies of the eye or associated with other systemic anomalies)
Juvenile glaucoma
(primary early-onset glaucoma)
Secondary glaucoma (commoner types listed below)
The short answer is no. In majority of patients glaucoma develops spontaneously but underlying risk factors as discussed above may play a contributory role. However, eating and living healthy always proves as an advantage in the long term for a number of health conditions.
Scientific evidence suggest that glaucoma eye drops are the single most beneficial medication that prevents the worsening of glaucoma. There is no scientific evidence to suggest that dietary supplements offer protection against glaucoma. However there is evidence that foods rich in anti-oxidants are good for overall general health including the health of your eyes. Below is a short list of some common foods with such benefits:

The normal eye pressure ranges between 10 to 21 mm Hg for most individuals. Your eye pressure can fluctuate up to approximately 5 points (measured in mm of Hg) during different times of the day. Eye pressure increases during night time, while lying down and can spike during early hours of the morning. In glaucoma patients this diurnal variation of eye pressure is more pronounced.
Yes, you can still drive provided you meet DVLA standards for driving (revised regulation for DVLA were implemented in 2013). However, patients with severe visual field defects in both eyes with advanced disease might be precluded from driving.
Group One (car drivers)
Standard 1: The minimum eyesight is 0.5 decimal (6/12) measured on the Snellen scale (with glasses), with both eyes together or, if you have only one eye with that eye. You must be able to read a car number plate at 20 metres.
Standard 2: The driver should have good peripheral vision on both sides and no significant defect in central vision. The DVLA states the need to have a binocular (both eyes together) horizontal field of vision of 120 degrees with not less than 50 degrees on each side of the centre and no significant field defect either within or encroaching onto the central 20 degrees of fixation.
Monocular vision: Those with sight with only one eye must meet the same criteria as above. If there is complete loss of vision in one eye then DVLA should be advised and driving can be restarted when the individual has been clinically advised that they have adapted to the condition.
Group Two drivers: Higher standards apply for those holding a LGV (lorry) or PCV (bus) drivers. Please check DVLA website (https://www.gov.uk/driving-eyesight-rules).
Responsibilities: It is the driver’s responsibility to advise DVLA of their condition but the medical profession also has a responsibility for public safety and is obliged to take action to inform DVLA if they know that driving is continuing without the driver advising DVLA.
Glaucoma and driving: Since early and moderate glaucoma affects the off centre parts of the field of vision and preserves the centre until late, most patients pass the DVLA driving eye test. The off centre peripheral damage can go unnoticed partly because the central vision is used most commonly and partly because one eye compensates for the other if the damage is in different areas of the visual field of each eye.
Glaucoma in one eye: For Group One drivers, if glaucoma is diagnosed in one eye and the other eye has a normal field of vision then it is not necessary to inform the DVLA at that stage. Group Two drivers need to inform the DVLA even if they have glaucoma in one eye since tests are more stringent for commercial drivers.
What happens when you advise DVLA of your eye condition? When a patient advises the DVLA of their eye condition, the DVLA writes back to the patient to carry out the DVLA sight tests (as above) in one of their approved centres. The results and a decision are then communicated directly to the patient in due course.